Abdominal pain can occur to due to many reasons- inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), some other health condition, or from eating something that didn’t sit well with your stomach. Regardless of the reason, experiencing stomach pain is both uncomfortable and distressing.
Chronic abdominal pain, on the other hand, can be a whole different story. Chronic pain — especially when it originates in your abdomen — can be more debilitating and have lasting effects on your brain. Any abdominal pain which lasts for about three months or more is labelled chronic.
Here we discuss the connection between chronic abdominal pain and your brain- and what you can do to find relief.
What is the Brain-Gut Connection?
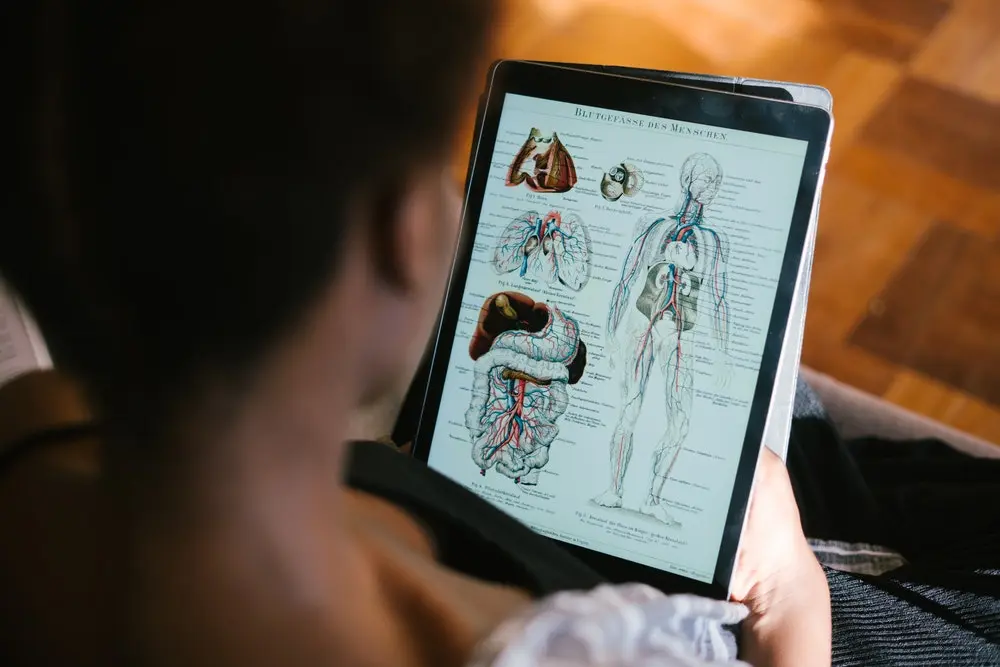
Our gastrointestinal tract, or gut, is sometimes described as our “second brain”. This is because the gut is controlled by its own complex nervous system comprising hundreds of millions of neurons. There’s a strong neurobiological connection between the brain and the gut, which may help explain why chronic abdominal pain — lasting longer than about three months — can be a major health problem.
This ongoing pain is often linked to psychological dysfunctions and can be explained by a malfunction of the communication between bowels and brain. According to estimates, one in five individuals suffers from recurring abdominal cramps, a sense of fullness, digestive problems or irritable bowel syndrome (IBS). The impact of chronic inflammatory abdominal pain can actually rewire your brain, eliciting a greater response. Many people with functional gastrointestinal (GI) disorders perceive pain more acutely than other people do because their brains are more responsive to pain signals from the GI tract. As this process continues, we suffer not just from the pain itself, but from our cognitive and behavioural reactions to it.
Behavioural changes are caused by colitis which is reflected in the limbic system and the connected regions of the cortex and chronic abdominal pain is often connected to psychopathologies. This can include anticipatory worrying about pain, inability to think about the future, and mood changes like irritability.
Traditionally, it was assumed that people with IBS or severe indigestion experienced anxiety and depressive episodes, as an underlying psychological disorder. But with new developments, it is observed that changes in the gut are actually driving anxiety experiences rather than the other way around.
One study observed that some people with IBS and anxiety have elevated levels of cytokines in their blood. Higher anxiety levels strongly correlated with higher cytokine levels. A similar study found that psychological distress can predict later onset of gut disorders and vice versa. An imbalance in these bacteria can affect the brain.
Altering gut bacteria is a new way to treat many diseases of the gut and possibly the brain, including through diets or by providing “good” bacteria and suppressing “bad” bacteria, that can be done with probiotics.
More studies are underway to understand the role of gut and pain in neurological diseases such as multiple sclerosis.
A research project funded by the Austrian Science Fund FWF has studied this concept and have made it increasingly clear that in case of abdominal pain, it is not only the neural pathways that are of significance but also hormonal and immunological signalling pathways.
How to Find Relief?
As we have seen, the gut microbiota has an impact on all sorts of bodily functions, including the brain and pain sensitivity, and also the individual’s mood. So, the first step in treating chronic abdominal pain is to get an understanding of the patient’s experience. Explaining your symptoms, types of episodes, location and severity, can help your doctor treating the pain appropriately.
Once the medical professional can understand how your pain is affecting them- there are two main treatment options you can go for- medications and behavioural therapy.
While taking drugs and medications can help make the pain go away, they won’t be a long term solution and making the pain go away completely.
Behavioural therapy aims to teach people strategies for coping with pain and discomfort and has been shown to be very effective in numerous research studies.
There are many different forms of behavioural therapy you can try.
- Cognitive behavioural therapy. This technique aims to refocus people’s thoughts negative thoughts, feelings, and behaviours related to their pain and trauma.
- Narrative exposure therapy. This form of therapy is usually conducted in a group setting, involving people sharing their experiences of pain and trauma. The goal is to reinforce the feeling empowerment
- Hypnotic techniques. This technique involves a broad array of techniques such as entering a trancelike state, focusing on your therapist’s suggestions about your emotions, thoughts, behaviours, and perceptions.
Talk to a medical health professional if you are experiencing symptoms of chronic pain, IBS or IBD.
Helping yourself through the pain and retrain your brain can also be helpful. Engaging in activities such as mediation, yoga, or doing things you enjoy can bring a sense of calm and distract you from the pain.